“Obesity is a chronic condition that affects a variety of systems that are also impacting employee productivity and medical costs.”
Lia Gass Rodriguez, MD, FAAP
Chief Medical Officer,
CVS Healthspire Payor Solutions
GLP-1s are one of the most talked-about topics in pharmacy benefits today – and with good reason. “GLP-1s” is common shorthand for a class of drugs that includes both glucagon-like peptide 1 receptor agonists and GIP/GLP-1s, which also target a second receptor, the glucose-dependent insulinotropic polypeptide receptor. Semaglutide, sold under the brand name Wegovy for weight management, is a GLP-1. Tirzepatide, sold under the brand name Zepbound for weight management, is a GIP/GLP-1.
Prior to their approval for weight loss, GLP-1s were effective options for treating type 2 diabetes. They have since emerged as powerful tools in our arsenal to combat obesity. Obesity affects more than 40 percent of U.S. adults and is linked to serious health concerns.3 Unsurprisingly, demand for these medications has surged. But drug manufacturers have set high list prices for them. GLP-1s may be just as well known for their high price as they are for their efficacy.
Utilization of medications in this class is sure to increase, especially as we discover more about their clinical potential. FDA-approved indications for semaglutide have already expanded to include cardiovascular (CV) event risk reduction. And tirzepatide is now approved to treat obstructive sleep apnea (OSA). Clinical trials are underway to evaluate these drugs’ potential for treating numerous other conditions.
This presents a clear challenge to plan sponsors who want to support their members in achieving better health without significant increases to drug spend or having to pass those costs down to their members in the form of dramatically increased premiums. Our approach to managing GLP-1s highlights how a PBM partner like CVS Caremark can help you manage costs while also promoting optimal health outcomes.
The science behind GLP-1s
Watch this video to learn about how GLP-1s help lower blood sugar and promote weight loss.
[Instrumental background music plays. Text description follows.]
How GLP-1s work
[CVS Caremark™ logo]
GLP-1 medications help lower blood sugar levels and promote weight loss.
GLP-1 medications are also called:
Glucagon-like peptide-1 agonists
GLP-1 agonists
Incretin mimetics
They influence different organs throughout the body, including:
Brain
Pancreas
Stomach
Liver
Heart
GLP-1s work by producing a synthetic version of a hormone released in the intestine when we eat - helping to regulate food intake and better control glucose.
They do this by:
triggering the pancreas to release more insulin
stopping the liver from making too much glucose
slowing down digestion, to feel fuller for longer
They're usually injectable medications, taken daily or weekly.
GLP-1 drugs are most effective when paired with proper dosing and lifestyle and diet changes.
At CVS Caremark, we're creating solutions that allow for a balanced approach to managing cost and care as this class of medications rapidly expands.
[CVS Caremark™ logo]
Let’s take a deeper dive into some considerations plan sponsors should keep in mind when determining their GLP-1 cost management strategy.
Obesity has long been linked to serious health conditions including type 2 diabetes, hypertension, hyperlipidemia, cardiovascular disease, osteoarthritis, various cancers, sleep apnea, depression and anxiety. And the prevalence is surging.
Thinking around obesity has shifted over the years. The American Medical Association officially recognized it as a chronic condition in and of itself in 2013.8 Given the individual and population health impact, it is our position that obesity should be addressed as proactively as other chronic conditions, with an evidence-based approach that can drive optimal health outcomes. To that end, we are in full support of offering coverage for weight management medications with cost and clinical controls in place.
Obesity costs U.S. employers and employees billions each year. Some of these costs are tied to medical expenses related to obesity and co-morbid conditions such as heart disease, diabetes, high blood pressure and even some cancers. There are indirect costs, too. Obesity has been linked to increased absenteeism, reduced productivity, disability and constraints on the labor force.9
Helping plan members access effective treatments, including weight management medication, could help offset these costs – and could boost employee recruitment and retention. It’s important to consider your benefit philosophy, employee demographics, turnover and other key indicators.
Weight management GLP-1s have been seen as gamechangers from a clinical standpoint, helping people shed significant weight when paired with lifestyle modification. Metabolic health affects nearly every facet of a person’s health and well-being. But the high price tags for these medications make coverage decisions challenging.
GLP-1s have the potential to help drive lifetime medical savings by reducing the risk for chronic conditions. However, these are longer-term effects that will take time. A recent analysis found that semaglutide and tirzepatide, at the current list prices, were the least cost-effective weight loss medications, when compared to naltrexone/bupropion (Contrave) and phentermine/topiramate.12 Another study found that even bariatric surgery is more cost-effective.13
Clearly there is a strong need for creative strategies to mitigate the high costs of these medications. We recommend a broad multilayered approach that includes lifestyle support such as through the CVS Weight Management™ program in coordination with other solutions you may have in place and alongside effective utilization management (UM) strategies to help ensure coverage is clinically appropriate.
Cost-effective coverage of weight management medications is possible. But it takes thoughtful consideration of how or if you will offer coverage, what tools you’ll have in place to help ensure your drug spend aligns with your coverage strategy, and effective ways you can empower your members to learn and put in practice the necessary lifestyle changes that are critical to achieving – and sustaining – better outcomes.
“Obesity is a chronic condition that affects a variety of systems that are also impacting employee productivity and medical costs.”
Lia Gass Rodriguez, MD, FAAP
Chief Medical Officer,
CVS Healthspire Payor Solutions
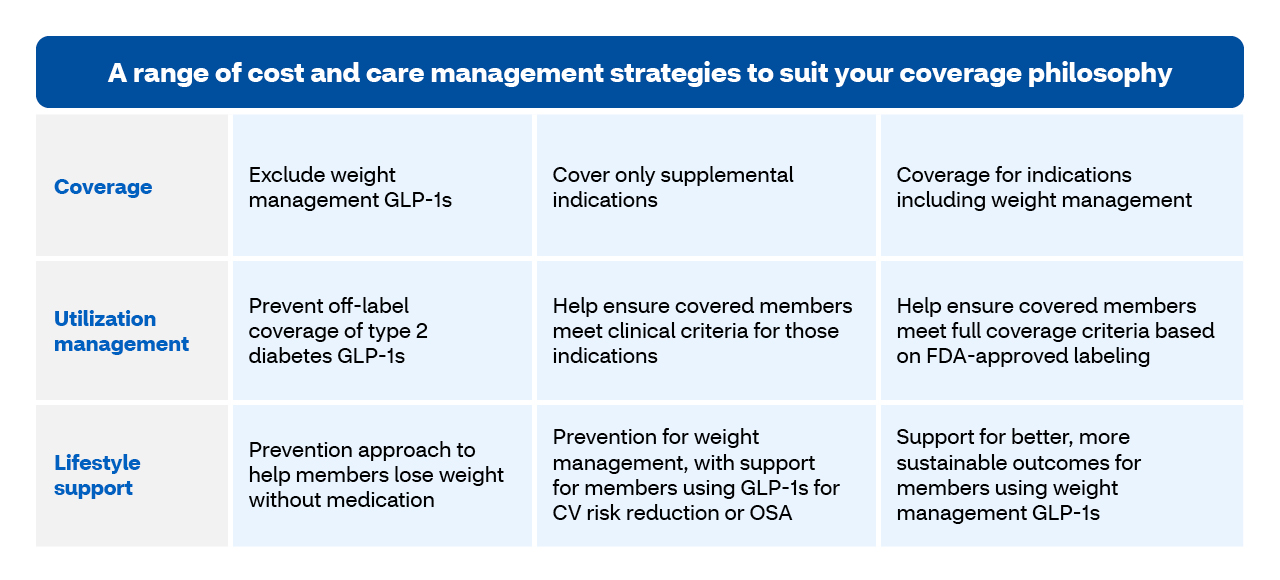
We start by meeting you where you are in terms of your organization’s coverage philosophy. You choose your level of coverage based on what works best for your business and the needs of your members.
Some plan sponsors may decide to align coverage with all FDA-approved labeling for weight management GLP-1s or to exclude the drug class altogether. Others may choose something in between – such as only covering these medications for supplemental indications, which currently include CV risk reduction and OSA.
Coverage considerations should take into account potential downstream effects of how addressing obesity could, over time, reduce medical spend related to comorbid conditions. You might also consider the impact to employee recruitment and retention, productivity and absenteeism, and potentially reducing the risk for on-the-job injuries
Once you’ve determined your coverage approach, it’s important to have the right UM controls in place to help manage costs in alignment with your coverage decision.
This is critical even if you choose to exclude weight management GLP-1s from coverage. For instance, prior authorization (PA), including our smart logic PA, can help prevent coverage of type 2 diabetes GLP-1s being prescribed off-label for weight management. Some plan sponsors may also choose to implement requirements for members to first try a less expensive weight management medication or to enroll in a lifestyle modification program before they can qualify for coverage.
Lifestyle changes are essential to achieving and sustaining a healthy weight – with or without medication. A metabolic health program such as CVS Weight Management, can provide wrap-around support to help your members who use weight management medications attain more significant and sustainable outcomes – and may even help some members meet their weight goals before even starting medication.
The program provides services and support well beyond digital-only solutions that promote a one-size-fits-all approach to diet. Our program support enrolled members with:
The program can seamlessly configure with your overall pharmacy benefit strategy to optimize efficiency and cost savings – with proven results from clients who have already implemented the program.
“Payors worry about the cost of these drugs. But they want to support better metabolic health for their plan members.”
Lia Gass Rodriguez, MD, FAAP
Chief Medical Officer,
CVS Healthspire Payor Solutions
Here are some examples of how our customizable weight management strategies have looked for some of our clients.
A large employer saw a sharp rise in claims for GLP-1s approved to treat type 2 diabetes among a member population of 150,000. The plan excluded weight management GLP-1s. But without UM edits in place, they couldn’t effectively prevent coverage of diabetes drugs used off-label for weight loss. We put in place a smart edit that screened PA requests for these medications, using information we already had about each member to look for a diagnosis code of type 2 diabetes or previous claims for diabetes medication or testing supplies. If criteria were met, the claim automatically approved. If not, it would require further review. The results? An 11-percent decrease in gross spend within just two months and 7,043 fewer users – with minimal disruption to members who had type 2 diabetes.
A large regional health system with about 40,000 employees was on track to spend more than $35 million on weight management GLP-1s. Since they had clinical resources, they were uniquely positioned to stand up their own weight management program. But they needed support to integrate it with their full benefits. We helped:
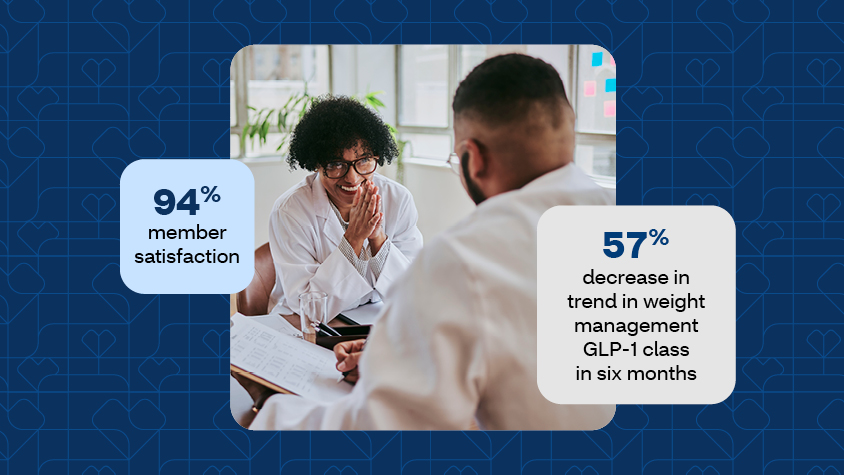
Through our combined efforts, they realized a 57-percent decrease in trend in the first 6 months in the weight management GLP-1 class alone – with 94 percent member satisfaction.
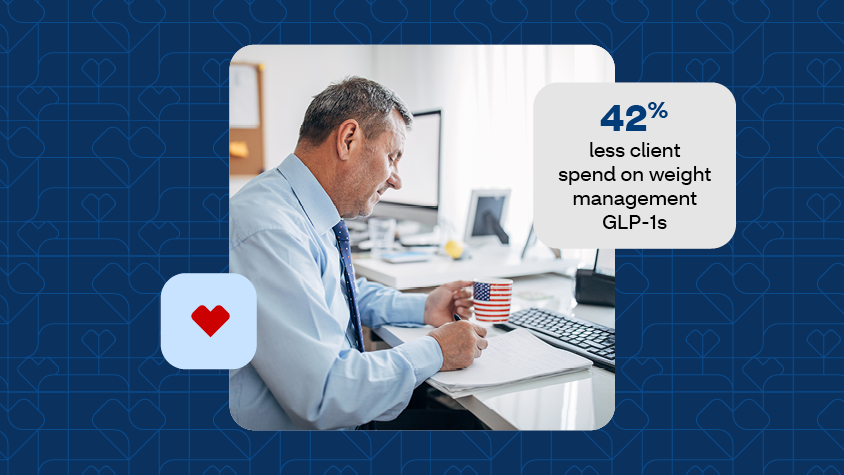
A government employer was facing high prevalence of obesity among their benefit plan members. They were seeing significant increase in spend related to weight management GLP-1s. After a different weight management program failed to deliver intended results, they turned to us for help. CVS Weight Management provided their members with tailored support to make lifestyle change and stay motivated. Plus, they got simplified and integrated program management – and 42% reduced spend on weight management GLP-1s.
“My quality of life has drastically changed. I’m much happier now and life is good! Thank you so much for all of your help.” – Enrolled member
We leverage the scale of our enterprise, a breadth of clinical and market expertise, and a deep understanding of your member population. We can help you build a strategy that makes sense for your organization and can integrate seamlessly with your pharmacy benefits.
Interested in learning more about our cost management solutions?