2022 Welcome Season
Maximizing satisfaction through service and operational excellence
Brian Leadingham, Senior Vice President of Client Service Operations

Each January 1 brings the opportunity to start fresh – to review, reflect and make resolutions for improvement in the coming year. At CVS Health, we make our resolutions long before January 1, during the months of planning that lead up to what is commonly known as Welcome Season. Although new plan members can begin to access their pharmacy benefits through CVS Caremark on the first of the year, much work is done in advance to ensure smooth transitions to keep members on track with their health.
This year, CVS Health welcomed 345 new clients and more than 4 million new members in our most successful Welcome Season ever. A significant number of clients – more than a thousand – also made changes to benefits. Implementing lessons learned from previous years enabled us to handle enormous volume while minimizing disruption and maximizing client and member satisfaction.
345 new clients
4M+ new members1
Changing PBMs can be challenging for some plan members, especially for those taking specialty medications, those with multiple chronic conditions or those who take several maintenance medications. Those members, who are identified through predictive modeling and a scoring index, may need extra support in the transition. As part of onboarding, we offer a unique, personal approach to help those members and minimize disruption.
99.92 percent of members had a seamless experience with no issues.2
High-Touch Outreach
Two weeks prior to transition, the High-Touch Outreach program begins with proactive phone calls to members with complex regimens. During these phone calls, we help them to transition their prescriptions, get started at mail or find an in-network pharmacy.
All commercial clients are automatically opted into High-Touch Outreach. During Welcome Season 2022, 70 percent of new clients had their eligible members contacted through High-Touch Outreach. The members contacted through the program this year had an average of seven prescriptions; and the initial phone calls lasted 30 to 35 minutes. Clearly, these are in-depth conversations. And members are highly satisfied: In a post-call survey, 88 percent said they are very confident that CVS Caremark will provide the support they need from their new PBM.
Looking ahead
We are building on and optimizing our digital connectivity to simplify client experience as we look forward to Welcome Season 2023 and the launch of myPBM.
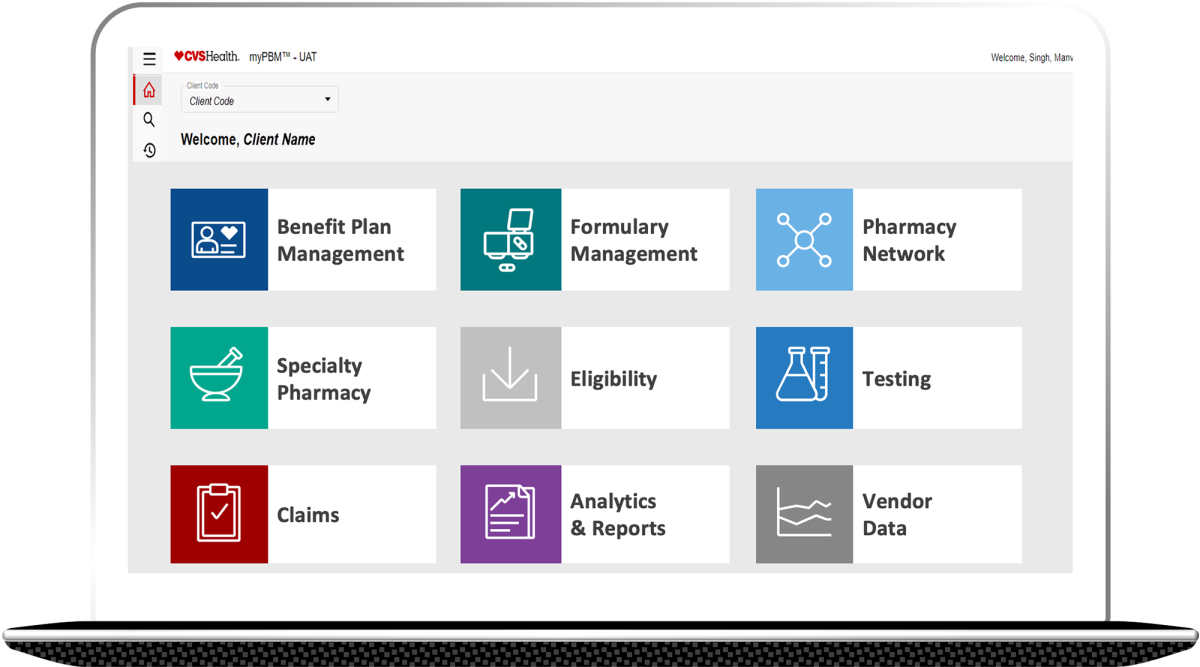
myPBM will enable end users – clients and business analysts – to gather requirements and track their status with an easy-to-use interface. It’s a one-stop shop for full pharmacy benefits management; clients can view, update and submit PBM requirements through a simple digital experience. Powered by a cloud-based platform leveraging modern architecture and technology through our new alliance with Microsoft, the solution will enable our powerful advanced analytics that use artificial intelligence to generate valuable insights.
CVS Health is committed to being clients’ best partner right from the start. Our relentless focus on service excellence means we don’t rest on our laurels; rather, we constantly look for ways to improve. We have invested in infrastructure, staff, systems and processes to make transitions simpler, smoother and less stressful. Every Welcome Season is an opportunity to provide the best client and member experience ever.